More Information
Submitted: December 03, 2020 | Approved: February 25, 2021 | Published: February 26, 2021
How to cite this article: Bell RN, Candilis PJ, Johnson NR. An update on outpatient competence restoration outcomes: The Washington DC Model. J Forensic Sci Res. 2021; 5: 001-006.
DOI: 10.29328/journal.jfsr.1001020
ORCiD ID: orcid.org/0000-0002-7172-364X
ORCiD ID: orcid.org/0000-0003-3594-8013
ORCiD ID: orcid.org/0000-0001-6649-1031
Copyright License: © 2021 Bell RN, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
An update on outpatient competence restoration outcomes: The Washington DC Model
Reston N Bell*, Phillip J Candilis and Nicole R Johnson
Department of Behavioral Health, Washington DC, USA
*Address for Correspondence: Reston N Bell, Ph.D, Department of Behavioral Health, Washington DC, USA, Email: [email protected]; [email protected]; [email protected]
This study provides an update to a previous study exploring time to restoration of adjudicative competence within an Outpatient Competence Restoration Program (OCRP). Authors examined the probability of restoration for individuals referred for outpatient competence restoration in the U.S. capital, and revisited the requirements of American Law, taking a closer look at how programmatic changes improve restoration and encourage adherence. Competence to stand trial remains a critical screening function of the judicial system to ensure that defendants have a basic understanding of courtroom procedures. Competency restoration is therefore an attempt to protect both the integrity of the system and the rights of defendants. Aggregate data from the OCRP’s previous four years of competence restoration efforts were reviewed for demographic characteristics, restoration rates, and time to restoration. Poisson regression modeling identified probability differences in restoration between sequential restoration periods. Since our initial analysis, the DC OCRP has been successful in restoring 97 of 345 participants (28.1%), with referral rates increasing from year to year. 39.2% are now restored after the 3rd round of competency restoration. Poisson regression modeling of individuals attaining competence during six successive restoration periods showed that differences for the first five rounds of restoration were not statistically significant (p = 0.418). In the 6th round, however, the difference in percentage of restored participants was statistically significant compared to previous rounds (irr = 0.32; p = 0.0001). We discuss the policy implications, especially those that suggest that the DC OCRP has improved its ability to restore competence beyond the 1st round of restoration.
As a function of United States law, outpatient competency education is provided to non-dangerous defendants who have been found incompetent to stand trial and who do not require inpatient hospitalization. Often referred to as the “Dusky Standard,” competency is defined by a landmark 1960 US Supreme Court case, Dusky v. United States, where a defendant’s right to a competency evaluation before proceeding to trial was codified [1]. Specifically, the court ruled that a defendant must have a “sufficient present ability to consult with his lawyer with a reasonable degree of rational understanding,” in addition to a “rational as well as factual understanding of the proceedings against him” [2]. The standard draws on fundamental principles of justice, establishing that it would be both unlawful and unethical for defendants to proceed in a criminal matter without having an understanding of the proceedings, its consequences, and the ability to assist their attorneys. Since its inception, there has been a wealth of scientific inquiry and opinion exploring the various tenets of the Dusky Standard [3,4], the populations for which it is appropriate [5], competency restoration, the assessment of competence [6], and the formulation of clinical opinion in relationship to it [7-9].
There are an estimated 25,000 to 39,000 competency evaluations conducted annually in the U.S. [10]. If defendants are deemed incompetent by a judge applying the Dusky standard, they may be committed to restoration on an inpatient or outpatient basis. While defendant adherence is at times a factor, dangerousness generally determines the setting. However, it is also governed by the resources of the state and the judgment of the fact-finder (i.e., the judge).
Since our initial report, with the exception of a pilot program in Minnesota and some “alternative” outpatient residential programming in a few states (Louisiana, Texas, Washington, Wisconsin, and Florida), the landscape of formalized restoration is unchanged. One alternative to traditional competency restoration programming can be found in Florida [11]. In response to increasing forensic psychiatric hospitalizations, the Miami-Dade Forensic Alternative Center was established. Some unique features of this program are that the defendant’s charges must be classified as a “minor felony,” and that programming may begin at an inpatient facility for stabilization and restoration. Subsequently, transfer to a secure residential treatment facility allows further treatment planning and community reintegration [11].
Although 35 states permit outpatient competence restoration, the number of formal programs remains at 16. Among the 16 states with outpatient restoration programs, there is notable variability in the standards for eligibility, the restoration curriculum itself, and clinician qualifications. For example, in Texas, the programs across the state have different eligibility criteria, and weigh factors such as criminal history, propensity for violence, and prior hospitalization differently [11]. Additionally, their programming appears to be based on the specific needs of the jurisdiction, so restoration looks different from county to county. One county, for example, utilizes state funding to support defendants with housing needs. In another county, the same funding is allocated for what is described as a “variety of non-competency related mental health services.” Restoration in New York State is only extended to individuals facing felony charges, a charge that generally carries a sentence of over a year in prison. Elsewhere, programs in Hawaii and Louisiana tend to limit OCR participation to defendants with misdemeanor or non-violent/dangerous charges [11].
Despite the variance in OCR models across the country, outpatient programming provides easily identifiable advantages over inpatient restoration. Services are conducted in a less restrictive environment, provide less infringement on personal liberty, are less disruptive to daily life, and are cost-saving for defendants and the public health system alike.
The DC OCRP
In the District of Columbia, any defendant can be ordered into restoration at the Outpatient Competency Restoration Program (OCRP), or on an inpatient basis at Saint Elizabeths Hospital, the District’s publicly funded secure psychiatric facility. The outpatient option adheres to the statutory requirement of the least restrictive alternative for mental health orders, but is not limited to defendants with misdemeanor offenses. The OCR program in Washington DC remains unique. It continues to serve individuals with both minor and serious offenses, as well as international defendants who break the law while visiting the city. Unlike some states, the DC OCR program does not have mandated medication compliance in the outpatient setting, but like many other programs it serves persons who are dually diagnosed or who meet criteria for intellectual disabilities.
The international visitors who become forensically involved often travel to the nation’s capital to communicate with government officials, Supreme Court Justices, security agencies, and the White House. Consequently, cultural competence is a critical component of local competency restoration. Consistent with the American Psychological Association’s recent practice guidelines, forensic practitioners are encouraged to acknowledge how past and present cultural experiences shape one’s engagement and willingness to access behavioral health services [13,14]. Similarly, in 2007 the American Academy of Psychiatry and the Law (AAPL) provided specific guidance on how areas such as “interviewing,” “acceptance,” “communication,” and clinician “cultural knowledge” can affect forensic evaluations [8].
One way that cultural competence has manifested itself in local service delivery is in interpreter services. A brief review of Spanish-language publications confirms that there are many different dialects, and indicates that ultimately, each country or region has its own unique sound [15,16]. Consequently, it is insufficient merely to arrange interpreter services; forensic educators must account for geographical location and years of formal schooling. In fact, one’s accent and cultural nuances of speech can also vary with socioeconomic privilege and setting. Not only have evaluators found that some forensic consumers (District terminology) have limited understanding of common translations, but that some legal terms do not directly translate into Spanish (e.g., Felony, Misdemeanor, and Not Guilty by Reason of Insanity).
Additional factors distinguish Washington DC’s OCR programming. Like Virginia, which has a standardized curriculum and set of criteria for all clinicians and counselors across the state, DC has developed a standardized curriculum and set of training criteria for service providers. While Virginia’s OCR programming is operated through their Community Service Boards, Wik’s write-up does not specify whether services are provided on an individual or group basis nor the frequency of these sessions (11).
From the outset, the DC model provides an intake and subsequent group restoration sessions for all forensic consumers. But restoration can deviate from this when group sessions appear ineffective and symptomology suggests that one-to-one restoration would be more effective. Although the DC program does not have the option of involuntary outpatient medication, counseling and alliance strategies help reduce symptoms, enhance retention, and improve restoration rates.
DC evaluators are board-certified forensic psychiatrists and forensically experienced psychologists who have either completed a forensic psychiatry fellowship or supervised experience with a trained clinician. This includes observing competency evaluations and then conducting at least five evaluations under the direct supervision of a fully certified and licensed clinician. Successful completion of this additional course of training provides acculturation to the program and its constituents, improved understanding of regulations, familiarity with local cultures and interpretations of law, and the proper thresholds for ascribing competence.
The DC OCRP meets at an outpatient clinic in the center of the District of Columbia. Participants are court-ordered to participate in restoration after having an initial screening and then a full competency evaluation by a psychologist to determine their suitability for the outpatient setting. Defendants charged with violent offenses, and who cannot be adequately managed in the community, are not recommended for the program. Disruptive behavior, poor program attendance or noncompliance with treatment recommendations resulting in disruptive symptomology are all reflected in updated reports to the court. However, the court ultimately determines whether the defendant continues in OCRP or if hospitalization is appropriate.
Restoration methods
Competence restoration is initiated with an intake session, where a program facilitator collects demographic information, and reviews the agreement that outlines expectations of program participants. Collectively, this information helps familiarize defendants with the limits of confidentiality, session offerings, attendance and participation policies, as well as the overall structure of the program. Since the time of the initial study, the number of available group sessions increased from twice to four days a week during the current study period, with the option of a morning and afternoon session on two of those days.
OCRP continues to increase session offerings. Participants now have the option of attending either a morning or afternoon session, Mondays through Thursdays. The expectation is that participants will attend one session each day. Additionally, to address the rational prong of the Dusky Standard (rational capacity), each participant is now allotted one individualized restoration session per cycle. The increased number of required sessions, the information provided during intake, and the individual restoration session were implemented with the intention of improving participant engagement and adherence to re-evaluation.
Previously, defendants reviewed what used to be the program’s primary teaching tool, a 42-question survey based on the Florida State Hospital CompKit. While most of the participants in the current study benefitted from the same tool, in the final year of data collection, the CompKit was further adapted in a series of detailed modules. These materials improved the individual’s factual understanding of the proceedings against them.
OCRP groups have been facilitated by a licensed clinical mental health provider, a master’s level social worker, and more recently a Ph.D. clinician with a Psychology Associate’s license. The facilitators use visual aids like a courtroom diagram, matching cards, word-finds, competency Jeopardy (like the US game show), and more recently a video that was specifically developed for District participants with intellectual limitations or who are visual learners 1. Facilitators make individualized determinations of how to supplement the curriculum with these activities.
__________________________________________________________________________________________________________ 1These materials are not publicly available so that attorneys and defendants do not gain unfair advantage before the formal assessment and restoration efforts. ___________________________________________________________________________________________________________During the course of restoration, mock trial hearings are conducted weekly in order to connect the participants’ daily education with real-life events. This remains an effective way to underscore the roles of courtroom personnel and procedure. When possible, Department of Behavioral Health legal counsel make themselves available for the mock trials. Additionally, the facilitator uses word association and acronyms to boost participants’ recollection. For example, introducing the concept of plea bargaining as a triangle, highlighting where it begins (offered by prosecutor), whom it is offered to and who has to accept it (defendant and defense attorney), and finally, who approves it (judge). Ultimately, the use of mnemonics and various teaching techniques accentuates the visual and kinesthetic elements of the program, strengthening participant learning. Such techniques include a newly developed multimedia computer-based set of modules consisting of simplified language and visual aids (shapes) to help forensic consumers identify relationships between various court personnel and procedures.
Upon completion of restoration, each defendant is assessed by a forensic evaluator after a period of 30-45 days (the typical length of a court order). If the court determines that additional restoration is necessary, defendants are re-evaluated every 30 days thereafter. Reports are generally written by the same examiner from cycle to cycle in order to maintain reliability, and to bolster familiarity with the nuances of the participant’s behavior.
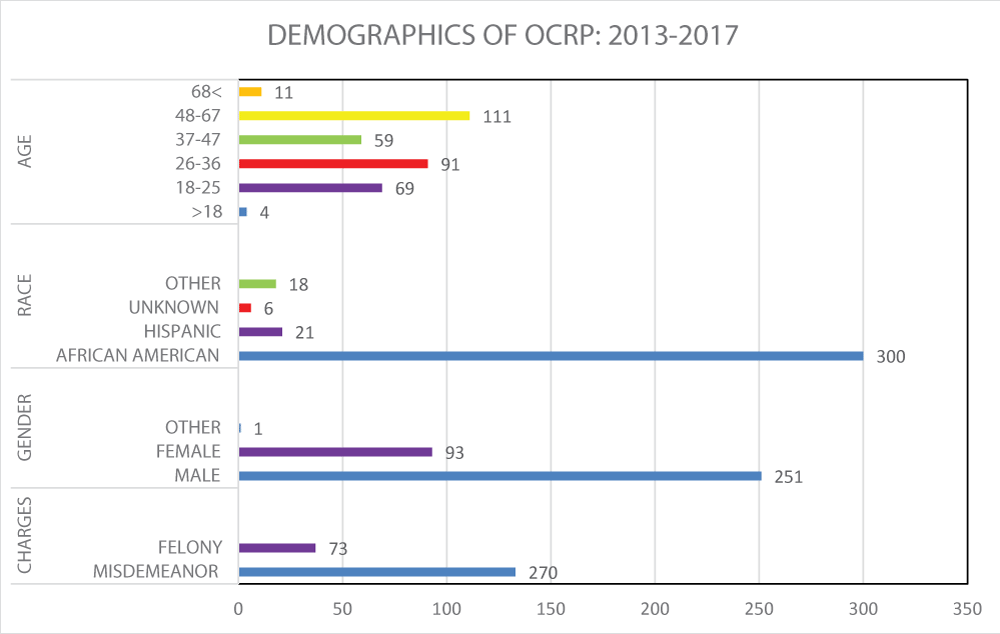
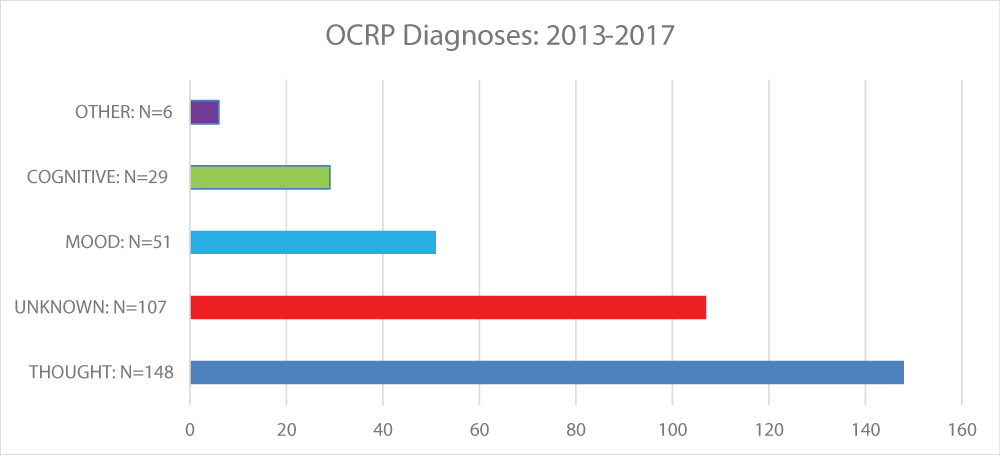
During the observation period, 2013 - 2017, the DC OCRP successfully restored 97 of 345 participants (28%). The number of individuals referred increased from 170 during the 2009 - 2013 study to 345. The percentage of forensic consumers restored dropped from 32% (2009 - 2013) to 28%. In the current study the difference between the rates of restoration for men (27.49%) and women (30.11%) were not statistically significant (p = 0.686). Overall, the demographics of the group in the current study are largely consistent with the participants in our previous study (Figures 1,2). Participants are still predominantly African American men with a mean age of 40 years. As before, most participants fell in the 48 to 67 year age range (32.17%). Additionally, a majority of participants, 79%, faced misdemeanor charges (78% in 2009 - 2013). Participants diagnosed with Thought Disorder as a primary diagnosis represent a majority of those ordered to OCRP, 43% (42% in 2009 - 2013).
Figure 1: Demographic of OCRP: 2013-2017.
*Due to missing data for some individuals, totals may not add to 345.
Figure 2: OCRP Diagnoses: 2013-2017.
A total of 345 defendants were ordered to participate in OCRP during the current observation period (2013 - 2017). 270 forensic consumers were ordered to participate in two or more rounds of restoration.
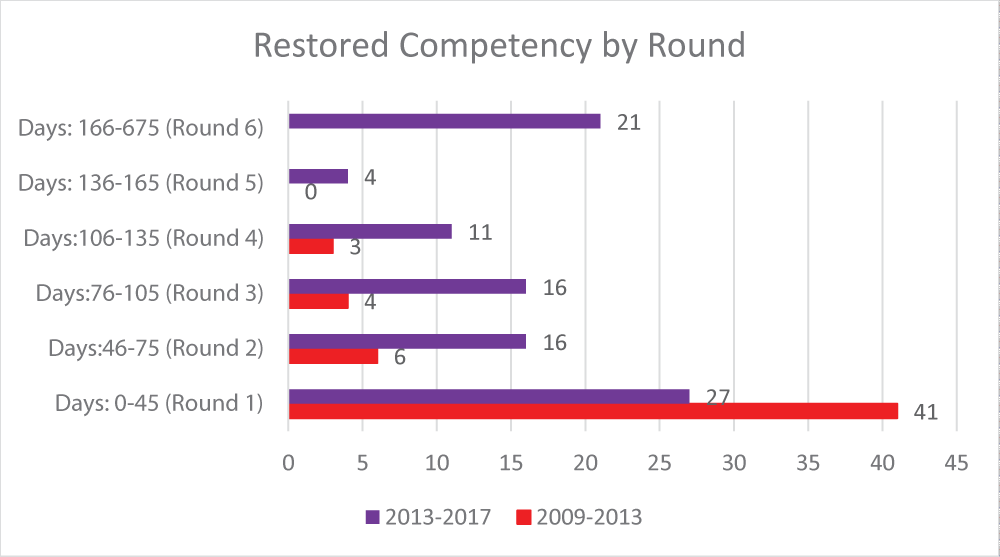
During the prior 2009 - 2013 study [17], the number of participants found competent to proceed dropped from 27 after the 1st round of restoration (45 days) to 16 after the 2nd round (75 days) (Figure 3). In that earlier study, a Jackson finding (i.e., the individual is unrestorable) was issued by courts after three or four rounds of restoration if competence had not been achieved. The judicial reasoning was that there was no substantial probability of competence for most people beyond that point. However, the current study shows that some persons were restored after five and even six rounds of restoration. Four individuals were restored after a 5th round (1%), and 21 after an extended sixth (6%). The 6th round spanned an extended period because some outliers were court ordered to participate without a specific return date. As such, they remained enrolled in the program until they were restored or their cases were dismissed.
Figure 3:Number of participants in different time periods restored from round to round.
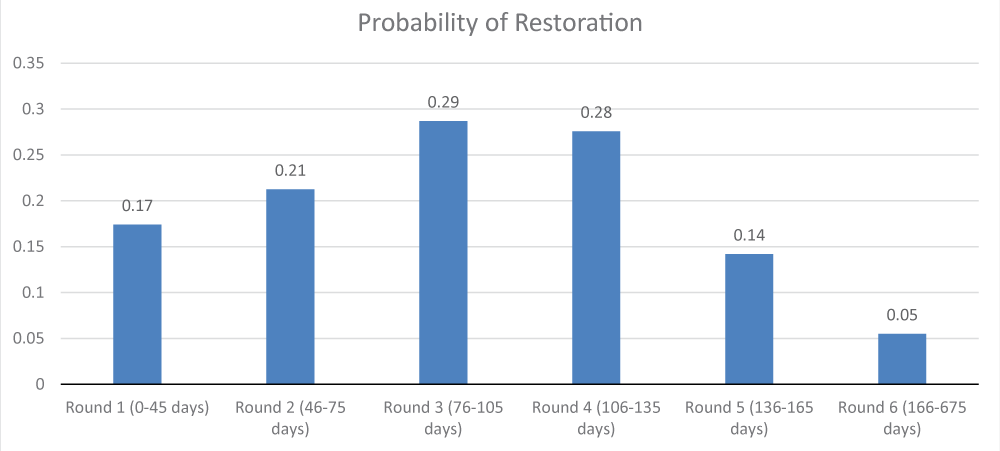
Although the number of persons restored in the first five rounds of this study appears to differ, the differences in restoration rates are not statistically significant from round to round (p = 0.418) (Figure 4). Poisson regression modeling allows for the comparison of restoration per day across each period. This provides the comparison of restoration percentages (per day of those identified as competent) against a published standard. For this study, the 1st round of restoration (0-45 days) was used as the standard against which each subsequent round was compared. This determination was informed by the findings of the earlier study [17], where a statistically significant number of participants was found competent by the end of the 1st round, the significance level was established at p < 0.05, and all reported significant results reflect this level of significance. Nonsignificant findings have the exact p - value noted in the text (e.g. p = 0.4) (Table 1).
Figure 4: Probability of Restoration.
| Table 1: Poisson model. | ||
| Factors: Indicator variables 0/1 | Incidence Rate Ratio (IRR) |
Significance (p - value) |
| Days 0-45 | Reference group | na |
| Days 46-75 | 1.22 | 0.53 |
| Days 76-105 | 1.65 | 0.11 |
| Days 106-135 | 1.59 | 0.2 |
| Days 136-165 | 0.82 | 0.7 |
| Days 166-675 | 0.32 | 0.0001 |
| Pseudo R-square = 0.60. The significance level was established at p < 0.05 and all reported significant results reflect this level of significance. Nonsignificant findings have the exact p - value noted in the text (e.g. p = 0.4). |
||
While the 6th round (166-655 days) does show that the lower percentage of restored participants differed statistically from the other rounds (irr = 0.32; p = 0.0001), the large number of days factored into the calculation, likely inflating its significance. The 6th round was analyzed by defining it as 166 to 365 days, at which point 19 of the 21 remaining participants were restored and the difference between all six rounds was no longer statistically significant (p = 0.15).
Changes made to the DC OCRP program appear to have had an effect in restoring competence beyond the initial 45-day period. Our initial 2015 investigation indicated that this was the most productive period for our competence program. Since our prior study, there have been changes in staffing, training, curriculum, as well as the number of required restoration sessions. These represent commitments of time and resources that were hypothesized to improve outcomes among those referred to a public sector restoration clinic. While we are unable to distinguish which of these changes has had the greatest impact, changes are detectable during the time spent in restoration. The demographic composition of the current set of participants is nearly identical to that of participants from the initial 2015 publication. One noteworthy departure is the age range of forensic consumers ordered to participate. There are a greater number of defendants below the age of 18 and above the age of 68 than there were previously.
This difference did not go un-noticed. In response to increasing numbers of juveniles being ordered to participate in OCRP, funding was obtained to develop additional programming and better meet the needs of this growing group of young defendants. Given the formal establishment of a juvenile restoration curriculum and programming, ultimately, there have been fewer underage forensic consumers ordered into the adult program. The greater number of forensic consumers over the age of 68 is indicative of those defendants from the original study that have begun to age out: the numbers of aging consumers in forensic programing has increased throughout the District.
This new data suggests that the program may have improved its ability to achieve restoration beyond the 45-day mark. Currently, the downward trend in restoration is not significant until the 6th round. This suggests that the program is able to restore competency consistently beyond the 1st round (45 days). Additionally, data indicates that our programming likely continues to restore defendants well into the 5th round of education. Although this supports the effectiveness of mainstream restoration efforts, especially after more resources are committed, it creates an option for keeping defendants within the forensic system. Indeed, this signifies a change in how long the courts are willing to keep defendants in restoration. In this jurisdiction, courts had previously ordered forensic consumers to inpatient treatment, dismissed, or issued a Jackson finding beyond the 4th round (135 days). Competency was deemed unlikely to be restored after this. The current review indicates that courts are now ordering continued restoration well beyond this mark (i.e., 655 days).
Of the 75 defendants ordered to return for a 6th round, 21 were successfully restored. A majority of individuals restored at this stage were diagnosed with thought disorders (n = 8), while others were diagnosed with no previous illness (n = 7).
Although this suggests an improved capacity to restore individuals who are severely mentally ill or who are newly diagnosed, it comes at a cost. Restricting a defendant’s liberty by requiring an almost two-year restoration may not be acceptable to a system that is responsible for protecting individual rights. The restoration period itself may be longer than any potential punishment. This, for many, is inconsistent with basic tenets of judicial fairness and requires a weighing of fairness to the individuals who must understand the system and the fairness of a protracted assessment.
Of the 29 persons within the Cognitive Diagnosis group, two of the three that were successfully restored to compe-tency, were restored in the 6th round. While it is commendable that restoration was achieved, the length of time is again significant. In fact, the low rate of restoration underscores the need for more specific resources for a group that is increasingly referred for restoration and yet is not easily restored. Given that the nature of the cognitive and developmental delays among this group of individuals tends to be fixed, it may be prudent to explore preventative programming that reduces their contact with the court system rather than making modifications to restoration programming. This suggests that changes in the availability of community-based support, activities, and supervision to supplement the needs of this population would be more advantageous and more ethical than efforts to adapt programming. With more individuals experiencing cognitive deficits in US forensic systems, this finding signals a greater need for methods that improve and shorten restoration for this vulnerable group.
Although barriers to speedy competence restoration persist across the United States, improvements in specific interventions can have an impact. A broader range of educational interventions is only one aspect of a forensic system that already seeks alternative placements for restoring its defendants. Further improvements in supporting forensic consumers with thought disorders and cognitive disabilities appear to be the next frontier in competence restoration. Partnerships with disability agencies are the next logical step. Any subsequent research that identifies the specific educational interventions that are most effective will enhance this movement toward a more collaborative and empirical competence restoration.
The authors are grateful to Roumen Vesselinov, PhD, for his review and oversight of the statistical analysis.
- Dusky v. U.S., 362 U.S. 402. 1960.
- Wik A, Hollen V, Fisher W. Assessment #9: Forensic patients in state psychiatric hospitals: 1999-2016. Alexandria, VA: National Association of State Mental Health Program Directors. 2017.
- Felthous AR. Competence to stand trial should require rational understanding. Journal of the American Academy of Psychiatry and the Law. Florida Senate. (2010). Interim report 2011-106: Forensic hospital diversion pilot program. Tallahassee, FL: Florida Senate. 2011. https://www.flsenate.gov/UserContent/Session/2011/Publications/InterimReports/pdf/2011-106cf.pdf
- Morris GH, Haroun AM, Naimark D. Assessing competency competently: toward a rational standard for competency-to-stand-trial assessments. J Am Acad Psychiatry Law. 2004; 32: 231-245. PubMed: https://pubmed.ncbi.nlm.nih.gov/15515910/
- Riggs Romaine CL, Kemp K, DeMatteo D. Evaluation of juvenile competency to proceed: Applying the Dusky standard. J Foren Psychol Practice. 2010; 10: 1-12.
- Heilbrun K, Rogers R, Otto RK. Forensic assessment. In Taking psychology and law into the twenty-first century. 2004; 119-146.
- Mossman D, Bowen MD, Vanness DJ, Bienenfeld D, Correll T, et al. Quantifying the accuracy of forensic examiners in the absence of a “gold standard”. Law Hum Behav. 2010; 34: 402-417. PubMed: https://pubmed.ncbi.nlm.nih.gov/19771499/
- Mossman D, Noffsinger SG, Ash P, Frierson RL, Gerbasi J, et al. AAPL practice guideline for the forensic psychiatric evaluation of competency to stand trial. J Am Acad Psychiatry Law. 2007; 35: S3-72. PubMed: https://pubmed.ncbi.nlm.nih.gov/18083992/
- Warren JI, Murrie DC, Stejskal W, Colwell LH, Morris J, et al. Opinion formation in evaluating the adjudicative competence and restorability of criminal defendants: A review of 8,000 evaluations. Behav Sci Law. 2006; 24: 113-132. PubMed: https://pubmed.ncbi.nlm.nih.gov/16557643/
- Miami-Dade Forensic Alternative Center Pilot Program Status Report. 2016.https://www.neomed.edu/wpcontent/uploads/CJCCOE_11_FACStatus.pdf
- Wik A. Alternatives to inpatient competency restoration programs: Community-based competency restoration programs. Falls Church, VA: NRI. 2018. https://www.nri-inc.org/our-work/nri-reports/alternatives-to-inpatient-competency-restoration-programs-jail-based-competency-restoration-programs /
- Danzer GS, Wheeler EMA, Alexander AA, Wasser TD. Competency restoration for adult defendants in different treatment environments.J Am Acad Psychiatry Law. 2019; 47: 68-81. PubMed: https://pubmed.ncbi.nlm.nih.gov/30737294/
- American Psychological Association. American Psychological Association ethical principles of psychologists and code of conduct. Washington, DC. American Psychological Association. 2017.
- American Psychological Association. Specialty guidelines for forensic psychology. Am Psychol. 2013; 68: 7-19. PubMed: https://pubmed.ncbi.nlm.nih.gov/23025747/
- Cameron R, Flores-Ferrán N. Perseveration of subject expression across regional dialects of Spanish. Spanish in Context. 2004; 1: 41-65.
- Hualde J. Spanish /i/ and related sounds: An exercise in phonemic analysis. Studies in the Linguistic Sciences. 1997; 27.
- Johnson NR, Candilis PJ. Outpatient competency restoration: A model and outcomes. World J Psychiatry. 2015; 5: 228-233. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4473494/