Research Article
Unrecognized myocardial infarction in the elderly

Haakon H Eilertsen2, Peer K Lilleng1, Bjorn Maehle1 and Inge Morild1*
1Department of Clinical Medicine, Faculty of Medicine and Dentistry, The University of Bergen, N-5021 Bergen, Norway
2Norwegian Naval Education and Training. P.O.Box 1 Haakonsvern K-38, N 5886 Bergen, Norway
*Address for Correspondence: Inge Morild, Department of Clinical Medicine, Faculty of Medicine and Dentistry, The University of Bergen, N-5021 Bergen, Norway, Tel: +47 55 97 25 60; Email: [email protected]
Dates: Submitted: 11 September 2017; Approved: 20 September 2017; Published: 22 September 2017
How to cite this article: Eilertsen HH, Lilleng PK, Maehle B, Morild I. Unrecognized myocardial infarction in the elderly. J Forensic Sci Res. 2017; 1: 077-086.
DOI: 10.29328/journal.jfsr.1001009
Copyright License: © 2017 Eilertsen HH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Forensic science; Ballistics; Propellant; MonoTrap; Chromatography
Abstract
This study presents the frequency of old myocardial infarctions (OMI), and the frequency of unrecognized myocardial infarction (UMI) in elderly people in a forensic material. It was also examined if predisposing factors of UMI could be identified. Of special interest was also to investigate the value of the police’s records as a source for medical information in a forensic setting. The study is based upon medico-legal autopsies of persons above the age of 60 at the time of death during the period 1999-2003. The study included 325 cardiovascular deaths. Of these, 166 died from OMI. UMI accounted for 123 of these (74%). Most UMI were located in the interventricular myocardial septum and left anterior wall (>60%), but no significant differences could be found between UMI and recognized MIs (RMI). No obvious reason could be found as to why the UMI remained unrecognized. Police records were inferior to the hospitals records, regarding medical information to the pathologist, with information about cardiac disease in about 60%, and with information about OMI in 11-17%. Hospital records supplying information about OMI were found in half the cases. It is concluded that unrecognized myocardial infarction is not uncommon among elderly persons, and with a high risk of sudden death. More emphasis should be put in recognizing OMI in ECGs to attempt to reduce the risk of sudden cardiac death.
Introduction
In previous studies of deaths among elderly persons in Western Norway, a high frequency of deaths from cardiovascular disease has been found [1,2]. These studies revealed many unrecognized cardiac diseases in the elderly population, especially unrecognized myocardial infarctions. The lack of a central heart registry in Norway made it difficult to confirm these findings. With a declining autopsy rate in Norway it was also difficult to confirm the findings [3,4]. Studies have shown that about 25% to 40% of myocardial infarctions are clinically unrecognized until detected with ECG performed for screening or other clinical purposes [5,6].
The risk associated with unrecognized myocardial infarction (UMI) has been demonstrated to be substantial, with a long-term total mortality as poor or worse than that of recognized myocardial infarction (RMI) [6]. It has been shown that the heart rate of ventricular tachycardia is inversely related to the size of dense myocardial scar [7]. The primary aim of the present study was to examine the frequency of UMI in a forensic autopsy material. Most similar previous studies have been on clinical series, and have investigated clinical aspects of symptoms and disease [5,6]. We also wanted to see if the localisation of the myocardial infarction (MI) had any relevance for whether the MI became recognized or remained unrecognized. As the study is based upon medico-legal autopsies requested by the police, we found it interesting to examine to what extent the police obtain information sufficient for the forensic pathologists before the medico-legal examination. The value of police reports as a source for clinical information was also of interest.
Materials and Methods
The material was collected from reports, based upon medico-legal autopsies at The Gade Institute, University of Bergen, during the 5 year period of 1999 through 2003. The inclusion criteria of the study were that the deceased was 60 years or older at the time of death, and that the death, after a medico-legal autopsy, was registered as caused by either an old myocardial infarction or an acute myocardial infarction. All abbreviations used in the text are listed in figure 1. Old myocardial infarction (OMI) was defined as a morphologically visible scar in the myocardium seen during the medico-legal autopsy, and confirmed microscopically as scar tissue in the myocardium. Acute myocardial infarction (AMI) was defined as morphologically acute changes seen microscopically with degeneration and necrosis of muscle fibres, infiltration of neutrophil granulocytes and contraction band necrosis.
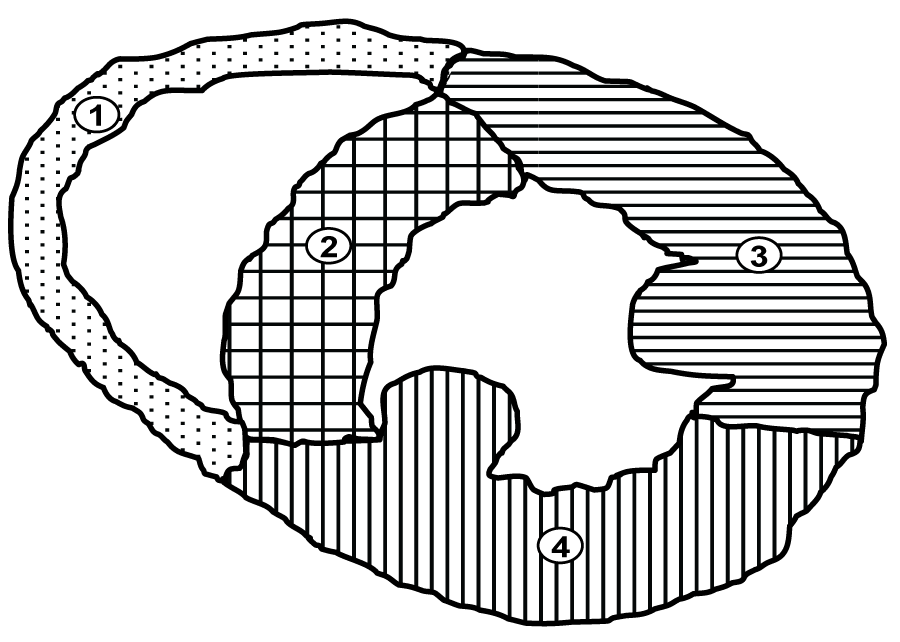
Unrecognized myocardial infarction (UMI) was defined as an infarction that was not clinically recognized, and therefore neither registered in the hospital records, nor in the police records, based on information from family and friends. Recognized myocardial infarction (RMI) was defined as MI that was documented either by information in the deceased’s hospital records, or by information from police, family and friends. The localisation of the myocardial infarctions (Figure 2), was registered together with heart weight. Body height and weight were used to calculate BMI. In addition, general information like day and month of death, marital status, accommodation, living arrangements and place of death of the deceased, were registered. The circumstances leading to the finding of the deceased, and information from the person who found the dead body, was also registered, from the police records.
Figure 2: Schematic drawing of transverse section through the heart. 1. Right ventricular wall; 2. Interventricular septum wall; 3. Left ventricular anterior wall; 4. Right ventricular posterior wall.
Medical information from health services
The local hospitals (Haukeland University Hospital, Voss County Hospital and Haraldsplass Deaconess Hospital), all medical records from the included cases were examined. Most patient records were from a period before the introduction of digital/electronically patient records, and full insight in the patients’ records was not always obtainable. We had, however, access to the ICD-9 or -10 codes given at the end of each admission, which was sufficient to register any serious cardiovascular condition. We did not register other diseases from the hospitals’ medical records.
Medical information from the police
With the police’s request of an autopsy, a report always follows describing the scene of death, the circumstances and some witness information. The police reports are based on interviews with healthcare personnel, friends and relatives. This information was registered to compare the quality of the police reports with the information found in the medical records from the hospitals. Some of the police reports also contain an inventory of medications found at the scene. These lists of medication could sometimes give an indication of the deceased’s medical condition. The Chi2 test and Student’s T-test was used in the analysis of the results. A probability level of p<0.05 was considered significant.
Results
There were performed 2425 forensic post mortem examinations in the period. There were 1169 patients 60 years or older. Of these 660 were autopsied. In the others, only an external examination was performed. Of the 660, 325 died from cardiovascular disease. In 46 patients an acute myocardial infarction was found and considered the cause of death. In 166 an old infarction was found and considered the cause of death. In the remaining 113 patients no infarction was found (Table 1). In 17 of the 46 patients dying from an acute MI, an old MI was also found in 15 men and 2 women. OMI constituted 51% of all cardiovascular deaths.
Table 1: The cause of death according to different type of heart condition in number of cases (%). No significant differences (p=0.6). |
|||
Cause of death |
Male |
Female |
Total |
Old MI |
130 (54) |
36 (43) |
166 (51) |
Acute MI |
31 (13) |
15 (18) |
46 (14) |
Coronary disease |
36 (15) |
13 (15) |
49 (15) |
Hypertrophic heart disease |
24 (10) |
4 (5) |
28 (9) |
Other acute conditions |
20 (8) |
16 (19) |
36 (11) |
Total |
241 |
84 |
325 |
Medical information from health services
From the 166 deceased (130 male and 36 female) with OMI revealed at autopsy (Table 2), 39 medical records (6 female and 33 male) could not be obtained. It was considered that no previous contact with the health services had taken place due to severe cardiovascular disease, for all of them, as all such known cases would have been admitted to the Haukeland University Hospital, with registration in the patient’s medical records. Thus the 6 females and the 33 males without medical records, but with an OMI revealed at autopsy, were considered as having an UMI.
| Table 2: Medical information from medical journals obtained from hospitals, and medical information obtained from police records. OR 1.81 for men, OR 2.28 for the women. Medical journals are a significant better source for medical information in sudden deaths than police reports. | ||||||
| Male | Female | |||||
| Info | RMI (%) | UMI (%) | Total (%) | RMI (%) | UMI (%) | Total (%) |
| Medical | 35 (27%) | 95 (73%) | 130 (100%) | 8 (22%) | 28 (78%) | 36 (100%) |
| Police | 22 (17%) | 108 (83%) | 130 (100%) | 4 (11%) | 32 (89%) | 36 (100%) |
Of the 30 females where a medical record was found, no information was found indicating an OMI in 22, while 8 of the females had a positive history of OMI. Medical records were obtained for 97 of the 130 males. Of these 97, 62 were without any medical history of an OMI, while among the remaining 35 males with medical records, positive information of an OMI was found. Thus, 33 males without, and 62 males with medical records were considered having an UMI, 95 males altogether (73 % of all male OMI). Similarly, 6 females without and 22 females with medical records were considered having an UMI, 28 altogether (78 % of all female OMI).
Medical information in the police records
Among the 36 females and 130 males with OMI, police records revealed information of symptoms like angina and cardiac failure indicating possible heart disease in 24 females (66.7%) and 72 (55.4%) males. There were no information in the police records of an OMI in 32 (89%) of the females, nor in 108 (83%) of the males. Not unexpectedly, the medical journals gave more information than the police records (Table 2). The police reports, however, gave information of 7 cases with an OMI, not recorded in any medical record, two female and five male cases.
Myocardial location of OMI
As many myocardial infarctions affected several adjacent areas in the myocardium at the same time, a number of combined infarctions were registered. The number of affected areas is therefore higher than the number of cases in the study. Only infarctions in the septum and in the left anterior- and posterior walls were found. The locations are given in Table 3. The healed myocardial scars were affecting a significant part of the ventricular walls, and no single subendocardial scars were registered. Among the 166 OMI, the septum was involved in 98 cases, the anterior wall was affected in 78 cases and the posterior wall in 42 cases (Table 3).
| Table 3: Location of all deaths from old myocardial infarctions, divided into UMI and RMI. No significant differences between UMI and RMI (p=0.101). In UMI the interventricular septum was affected in 72 of the 123 cases (59 %), the left anterior wall in 54 cases (44 %) and the left posterior wall in 32 (26 %). In RMI the septum was involved in 26 of the 43 cases (60 %), the left anterior wall in 24 (56 %) and the left posterior wall in 10 (23 %). | ||||||
| OMI | ||||||
| Myocardial infarction location | UMI |
RMI |
||||
| Male | Female | Total | Male | Female | Total | |
| Septum | 23 | 11 | 34 | 10 | 0 | 10 |
| Septum-Anterior | 25 | 5 | 30 | 12 | 3 | 15 |
| Septum-Posterior | 7 | 1 | 8 | 1 | 0 | 1 |
| Anterior | 6 | 3 | 9 | 2 | 0 | 2 |
| Anterior-Posterior | 13 | 2 | 15 | 4 | 3 | 7 |
| Posterior | 7 | 2 | 9 | 1 | 1 | 2 |
| Other | 14 | 4 | 18 | 5 | 1 | 6 |
| Total | 95 | 28 | 123 | 35 | 8 | 43 |
In UMI the septum was affected in 72 of the 123 cases (59 %), the left anterior wall in 54 cases (44 %) and the left posterior in 32 (26 %). In RMI the septum was involved in 26 of the 43 cases (60 %), the left anterior wall in 24 (56 %) and the left posterior in 10 (23 %). Due to the many combined infarctions, the number of infarcted areas was 242 in the 166 cases with OMI. The myocardial interventricular septum was the most frequent localisation of the OMI in this study. Hearts with multiple scars from OMIs, where the location of the scars were not clearly identified in the autopsy report, or where substantial scarring was a histological finding, were classified as “other location”. Significant difference in localisation between UMI and RMI were found (p=0.030, OR 0.81(0.67-0.98)).
Acute myocardial infarctions
In 46 cases, the cause of death was considered to be an AMI. There were 15 females and 31 males (Table 4). Among the 31 males, 15 had an OMI in addition to an AMI, but only two of these OMIs were recognized (RMI). Two of the 15 females with AMI also had OMI, while one of the two females with AMI had a RMI. Most AMI were located in interventricular septum (23 of the 58 locations) followed by anterior wall infarctions (21 of 58 locations).
| Table 4: All patients with AMI as the cause of death, with location of OMI and AMI in the same hearts. | ||||||
| Location | Acute MI |
Old MI |
||||
| Male (%) | Female (%) | Total (%) | Men (%) | Female (%) | Total (%) | |
| Septum | 9 (29) | 5 (33) | 14 (30) | 8 (26) | 0 | 8 (47) |
| Septum-Anterior | 7 (23) | 2 (13) | 9 (20) | 2 (7) | 1 (7) | 3 (18) |
| Septum-Posterior | 0 | 0 | 0 | 0 | 0 | 0 |
| Anterior | 7 (23) | 2 (13) | 9 (20) | 1 (3) | 0 | 1 (6) |
| Anterior-Posterior | 1 (3) | 2 (13) | 3 (7) | 2 (7) | 0 | 2 (12 |
| Posterior | 6 (19) | 2 (13) | 8 (17) | 1 (3) | 0 | 1 (6) |
| Other | 1 (3) | 2 (13) | 3 (7) | 1 (3) | 1 (7) | 2 (12) |
| Total | 31 | 15 | 46 | 15 | 2 | 17 |
Age, gender, body mass index, and heart weight
In the males, weight could not be obtained due to decomposed body in two cases. Results for all groups are shown in table 5. No significant differences between the groups were found. The mean heart weight was elevated for all groups. The heart weight was on average 0.66 % of the bodyweight.
| Table 5: General statistics on those with cause of death OMI vs AMI. The table shows the mean (±SD) and range. No significant findings between male and female with Students T-test. | ||||
| Old myocardial infarctions | Acute myocardial infarction | |||
| Male | Female | Male | Female | |
| Age (year) |
71±8 (60-93) |
75±9 (62-94) |
70±7 (60-85) |
76±7 (69-90) |
| Height (cm) |
177±7 (163-198) |
163±7 (146-176) |
175±9 (148-194) |
161±9 (141-175) |
| Weight (kg) |
83±18 (43-159) |
68±17 (46-126) |
79±14 (52-114) |
70±13 (42-85) |
| BMI | 26±5 (15-52) |
25±5 (19-47) |
26±3 (20-35) |
26.6±4 (17-33) |
| Heart weight (gram) |
570±151 (280-775) |
458±151 (280-685) |
515±89 (380-720) |
448±115 (300-760) |
Living arrangements, accommodation and factors related to the discovery
Most females lived alone, while a greater proportion of the males lived with a partner (p<0.05). A significant difference in residence was found between females who tended to live in apartments, and males who tend to live in detached or semidetached houses (p<0.05). No significant differences between males and females could be found regarding who found the deceased, but a greater amount of men was found by friends and co-workers. More males (31%) were also observed getting ill, than females (16%), although no significant differences could be found (Table 6).
| Table 6: Living arrangements, the cause of finding and by whom, in those dying from OMI. | ||||
| Female | Male | Total | ||
|
Marital status (p=0.010) |
Unknown | 3 | 12 | 15 |
| With partner | 5 | 52 | 57 | |
| Alone | 28 | 66 | 94 | |
| 36 | 130 | 166 | ||
|
Residence (p=0.002) |
Unknown | 5 | 54 | 59 |
| Detached/Semidetached | 8 | 36 | 44 | |
| Apartment | 21 | 37 | 58 | |
| Institution | 2 | 3 | 5 | |
| 36 | 130 | 166 | ||
|
Found by whom (p=0.105) |
Unknown | 3 | 20 | 23 |
| Family | 18 | 51 | 69 | |
| Health workers/Police | 13 | 28 | 41 | |
| Friends/co-workers | 2 | 26 | 28 | |
| Other | 0 | 5 | 5 | |
| 36 | 130 | 166 | ||
|
Found why (p=0.103) |
Unknown | 4 | 13 | 17 |
| Observed getting ill | 6 | 40 | 46 | |
| Family came home | 1 | 1 | 2 | |
| Not appeared at work | 3 | 5 | 8 | |
| Not answering phone | 4 | 14 | 18 | |
| Routine visit | 11 | 17 | 28 | |
| Other | 7 | 40 | 47 | |
| 36 | 130 | 166 | ||
Discussion and Conclusion
The material is based upon forensic examinations, and most cases from the study population were found dead outside a health institution, most of them at home. Other studies have also shown that a high proportion of fatal cardiac arrests occurred outside hospital and that an inverse relation with age exists [8,9]. In one study, 91% of such fatalities in persons below age 55 and 70% at age 65-74 happened outside hospital [8]. A similar age trend has been reported from the United States on the basis of data from death certificates and was also observed in the pilot Brighton heart attack study [10,11]. The high proportion of deaths outside hospital shows the potential limitations of further improvements in hospital treatment. To reduce the number of sudden cardiac death, primary prevention and intervention before admission is necessary. This can be improved by intensified training of ambulance crew members, and also by public education in cardiopulmonary resuscitation and defibrillation. Implantable cardioverter defibrillators (ICD) can also prevent sudden deaths, and it is therefore important that UMIs can be recognized.
Depending on the country’s rate of medico-legal autopsies, a forensic autopsy material will give more information about the cardiac health in general elderly population than a hospital autopsy material. The mortality rate from cardiac disease in Norway declined during 1987 to 2007 [12]. A decline in the number of myocardial infarctions was also seen during the (19)90ies. New clinical diagnostic guidelines, with the measurement of troponin as a blood test from around year 2000, led to an increase of 33 % more MIs during 2000-2002 [13]. Some of our UMIs, might have been detected clinically with these diagnostic guidelines. UMI are very common also in other studies, and beyond age 65, women are as vulnerable to cardiovascular death as men [14]. UMI pose a high risk of sudden death with 34% of sudden deaths attributed to UMI in one study from USA [15].We found a higher proportion of UMI in sudden deaths, but the American study is conducted after the implementation of the new diagnostic guidelines. With the use of such new diagnostic guidelines, the number of UMIs in our population might have been lower.
Clinicians and pathologists differ in the definition of the anatomic location of the myocardial infarction. Clinicians often define the location from ECG or echocardiography findings. These may differ from the anatomical classification the pathologists use. One clinical study, performed with MRI and nuclear contrast imaging, showed that 49 % of all MI, were in the left anterior wall, and the rest in other locations [16]. Our findings indicate a different distribution of the MIs, with the interventricular septum being more often involved, but direct comparisons is difficult due to differences in nomenclature. A Norwegian study gives the distribution of coronary atherosclerosis, and thus an indication where one could suspect to find AMI [17]. However, the blood supply to the interventricular septum can derive from different major vessels. The right coronary artery (RCA) or the left circumflex artery (CX) and in some cases both, can all supply the right posterior descending (PDA) artery. In addition, the anterior aspect of the septum is supplied by the left anterior descending artery (LAD). In the study referred, LAD was affected in 44% of the cases, CX in 14% and RCA in 41% of the patients. Only 20% had a 3-vessel coronary disease. 55% had a single vessel disease. In our study, more patients had 3 vessel disease. We found no differences in symptoms reported, between patients with UMI and RMI, and were not able to detect a difference between UMI and RMI that could explain why some MIs remain unrecognized.
In one study individuals in lower socio-economic groups had fewer visits to a doctor, less medication and were less likely to have cardiac disease prior to death [18]. We found no significant differences when considering socio-economic factors such as marital status and type of residence. In this study from Finland, of medico-legal autopsies, the interventricular septum was involved in 52% of all OMI, not unlike our results [18].
The septum was equally often affected in UMI and RMI. The anterior wall was more often affected in RMI than in UMI, which is similar to other studies where this finding was significantly more common in patients with RMI than in UMI [19]. Posterior wall infarction was equally often seen in UMI and RMI, while posterior infarction was more common in UMI than RMI in this study from USA [20]. Compared with the patients with clinically recognized acute myocardial infarction, the patients with clinically unrecognized infarction had a significantly higher incidence of diabetes mellitus. This has not been examined in the present study.
Other studies have shown a ratio as low as 5% for silent ischemia in elderly [20]. Elderly persons may have atypical symptoms and be more prone to silent myocardial ischemia [21]. As the mean age in our study was high, this could explain our findings of a high number of OMI, although the reason why elderly have atypical symptoms is not known. In some studies of UMI, very few had ECGs indicating OMI, with ECG having low sensitivity [22,23]. A complicating factor in the diagnosis of OMI is that a random ECG may not always give indications of OMI. A study regarding infarctions in the septum, showed that the Selvester QRS points system indicated a 52 % prevalence in anteroseptal scarring, but only one of 46 patients involved, had septal scarring [24]. Random ECG is difficult to use in the diagnosis of UMI, as Q-waves have poor predictive value of localisation of MI in all parts of the heart, except the anterior wall, where one finds a scar in 89% of all Q-waves [25].
Studies have shown that in patients with cardiac ischemia and OMI, there can be changes in the potassium ion channels that may predispose to cardiac conduction disturbances, and may cause cardiac arrhythmia [26]. Old myocardial infarctions can cause delayed conductivity, and thus arrhythmia, especially if it is interfering with the bundle of His [27]. The present study is pathology based, and for an AMI to be visible microscopically, the patient has to survive the AMI for several hours. Therefore, in this study, we cannot exclude that in addition to the registered OMIs, there also can be some AMIs. A number of the deaths have been witnessed, and the general impression is that the death is very sudden. The myocardium has been thoroughly examined microscopically before we have concluded that a diagnosis of AMI is not possible. Biochemical markers have not been used. We are convinced that malignant arrhythmias occur in OMI and that therefore the cause of death is the OMI and in most cases not an AMI.
The heart weight was high for most of the patients in our study, with a ratio of 0.66% of bodyweight. It is well known that sudden cardiac deaths have been associated with increase in myocardial mass [28,29]. In our material the mean heart weight was enlarged, with 0.66% of bodyweight, a risk factor of sudden deaths, although no significant differences could be found between UMI and RMI.
The police records were nearly as good as the medical records for information regarding pre-mortal state of health in this study. Compared to how often cardiac disease is found during a post-mortem, we found that a large number of heart conditions were unknown in the police records, but also to a high degree unknown in medical records. In a study from New Zealand, with evaluation of police reports in sudden unexplained death, more than 75% of the police reports did not contain necessary information of medical or family history [30]. Our impression is that the police reports in Western Norway probably were a reasonable good source of information.
The police reports are, however, not as good a source of information as the medical journal. In some cases, the police reports are scarce, due to lack of relatives to ask, or other circumstances making a full interview difficult. However, it is obvious that information found in the medical journals, hopefully known to the deceased, has not been shared with the relatives, making them unfamiliar with the deceased’s health status.
The study population has been found to differ very little from the average population in Western Norway [3,4,31,32]. No significant differences were found regarding pre-mortal state of health, living arrangements and type of residence. No more diseases or ailments, no high risk factors for sudden deaths, or severe illness than in the average population were found.
No seasonal differences, relating to age, sex or origin of MI were found. There were not found any increase in the death rate during the influenza season, or during warmer periods in the summer when elderly have had a higher risk of lethal illness [33,34]. In this forensic material from a Western Norwegian population of sudden cardiac deaths, half of the decedents probably were unaware of their survived previous myocardial infarction. Most of these unrecognized conditions were probably silent infarctions. The anatomical localisation of the UMIs, was mostly in the myocardial interventricular septum. Males had more UMIs than females, and males were younger than females. Unfortunately it was not stated in the forensic journals if the OMI was transmural. This could be of importance as it has been shown that the correlation between the heart rate of ventricular tachycardia increases with higher degree of scar transmurality [7]. Such information could be used when selecting candidates for ICD. There were no significant correlation between the location of the MI and the lack of symptoms. The mean heart weight was elevated, and all victims had severe coronary disease. Most of the decedents died outside health institutions.
To reduce the number of sudden cardiac death it is necessary to inform the public about symptoms of a MI. To reduce the death among those who have an UMI, it is necessary with intervention by intensively trained ambulance crew members, and also by public education in cardiopulmonary resuscitation and defibrillation.
New advances in clinical diagnostics of myocardial ischemia have been introduced since the study population was examined. Today’s frequency of UMI may be different. A combined study of medico-legal autopsies and clinical autopsies may reveal if the last decade’s new diagnostic guidelines, as well as new diagnostic methods such as coronary computed tomography, and frequent use of angiography have reduced the frequency of UMI.
References
- Eilertsen HH, Lilleng PK, Maehle BO, Morild I. Unnatural death in the elderly. A forensic study from western norway. Forensic Sci Med Pathol. 2007; 3: 23-31. Ref.: https://goo.gl/aJzqPz
- Eilertsen HH, Lilleng PK, Maehle BO, Morild I. Death in the Elderly. Scand J Forensic Sci 2005; 1: 15-9.
- Lindström P, Janzon L, Sternby NH. Declining autopsy rate in Sweden: a study of causes and consequences in Malmö, Sweden. J Intern Med. 1997; 242:157-165. Ref.: https://goo.gl/2Z7SEm
- Berget E, Ramnefjell M, Svendsen EB, Bertelsen BI, Maehle BO, et al. Decline in hospital autopsies. Tidsskr Nor Lægeforen. 2007; 127: 2800-2802. Ref.: https://goo.gl/4Hg7Xh
- Sheifer SE, Manolio TA, Gersh BJ. Unrecognized myocardial infarction. Ann Intern Med. 2001; 135: 801-811. Ref.: https://goo.gl/71MWz3
- Sheifer SE, Gersh BJ, Yanez ND, Ades PA, Burke GL, et al. Prevalence, predisposing factors, and prognosis of clinically unrecognized myocardial infarction in the elderly. J Am Coll Cardiol. 2000; 35: 119-126. Ref.: https://goo.gl/GLViod
- Woie L, Eftestøl T, Engan K, Kvaløy JT, Nilsen DW, et al. The heart rate of ventriculartachycardia following an old myocardial infarction is inversely related to the size of scarring. Europace. 2011; 13: 864-868. Ref.: https://goo.gl/sgNQG6
- Norris RM on behalf of the United Kingdom Heart Attack Study Collaborative Group. Fatality outside hospital from acute coronary event in three British health districts, 1994-1995. BMJ 1998; 316: 1065-1070. Ref.: https://goo.gl/vTJbxp
- Task Force Report. The pre-hospital management of acute heart attacks. Recommendations of a Task Force of The European Society of Cardiology and The European Resuscitation Council. Eur Heart J. 1998; 19 1140-1164. Ref.: https://goo.gl/g3hY85
- Gillum RF. Sudden coronary death in the United States 1980-1985. Circulation. 1989; 79: 756-65. Ref.: https://goo.gl/sVRnCt
- Norris RM, Dixon GF, Chamberlain DA, Vincent R. Mortality from ischaemic heart disease outside and inside hospital: the Brighton heart attack study. Br Heart J. 1994; 71: 33.
- Reikvam Å, Hagen TP. Endringer i dødelighet av hjerteinfarkt. Tidsskr Nor Legeforening. 2011; 131: 468-470. Ref.: https://goo.gl/m3N5Wp
- Hagen T, Reikvam Å. Marked increase of the number of myocardial infarctions following introduction of the new diagnostic criteria. Tidsskr Nor Lægeforening. 2003; 123: 3041-3043. Ref.: https://goo.gl/957d6S
- Kannel WB, Vokonas PS. Demographics of the prevalence, incidence, and management of coronary heart disease in the elderly and in women. Ann Epidemiol. 1992; 2: 5-14. Ref.: https://goo.gl/Ms643X
- Adabag AS, Peterson G, Apple FS., Titus J, King R, et al. Etiology of Sudden Death in the Community: Results of Anatomic, Metabolic and Genetic Evaluation. Am Heart J. 2010; 159: 33-39. Ref.: https://goo.gl/bkTZyZ
- Masci PG, Ganame J, Francone M, Desmet W, Lorenzoni V, et al. Relationship between location and size of myocardial infarction and their reciprocal influences on post-infarction left ventricular remodelling. Eur Heart J. 2011; 32: 1640-1648. Ref.: https://goo.gl/yqw6CB
- Kløw N-E, Bendz B, Eritsland J, Hoffman P, Stavnes S, et al. Angiographic results of primary angioplasty in acute myocardial infarction. Tidsskr nor Lægeforen. 2001; 121: 780-783. Ref.: https://goo.gl/Y5GWPi
- Rissanen V, Romo M, Sarna S, Siltanen P. Deaths from ischemic heart disease in persons aged 65 or younger in Helsinki in 1970 with special reference to patho-anatomic findings in hearts.? 211. Acta Med Scand 1975; 197: 51-60. Ref.: https://goo.gl/xFQNFY
- Cabin HS, Roberts WC. Quantitative comparison of extent of coronary narrowing and size of healed myocardial infarct in 33 necropsy patients with clinically recognized and in 28 with clinically unrecognized ("silent") previous acute myocardial infarction. Am J Cardiol 1982; 50: 677-681. Ref.: https://goo.gl/oXesFC
- Valensi P, Lorgis L, Cottin Y. Prevalence, incidence, predictive factors and prognosis of silent myocardial infarction: a review of the literature. Arch Cardiovasc Dis. 2011; 104: 178-188. Ref.: https://goo.gl/VCYocs
- Haze K, Oka T, Sumiyoshi T, Itagane H, Endo C, et al. Acute myocardial infarction and silent myocardial ischemia in the elderly--clinical features and effectiveness of therapy in an era of coronary intervention. Nippon Ronen Igakkai Zasshi. 1996; 33: 346-352. Ref.: https://goo.gl/RqVt65
- Gerbaud E, De Clermont-Galleran H, Erickson M, Coste P, Montaudon M. Cardiac MRI for Detection of Unrecognized Myocardial Infarction in Patients With End-Stage Renal Disease: Comparison With ECG and Scintigraphy. American Journal of Roentgenology 2009; 193: 25-32. Ref.: https://goo.gl/CLtuRX
- Schelbert EB, Cao JJ, Sigurdsson S, Aspelund T, Kellman P, et al. Prevalence and prognosis of unrecognized myocardial infarction determined by cardiac magnetic resonance in older adults. 2012; 308: 890-896. Ref.: https://goo.gl/UynMPK
- Siddiqui AM, Samad Z, Crowley AL, Hakacova N, Harrison JK, et al. Relationships between cardiac magnetic resonance imaging abnormalities in the inter-ventricular septum and Selvester QRS scoring criteria for anterior-septal myocardial infarction in patients with right ventricular volume overload. J Electrocardiol. 2013; 46: 256-262. Ref.: https://goo.gl/TY9C4h
- Rovai D, Di Bella G, Rossi G, Lombardi M, Aquaro GD, et al. Q-wave prediction of myocardial infarct location, size and transmural extent at magnetic resonance imaging. Coron Artery Dis. 2007; 18: 381-389. Ref.: https://goo.gl/guikst
- Näbauer M, Kääb S. Potassium channel down-regulation in heart failure. Cardiovasc Res. 1998; 37: 324-334. Ref.: https://goo.gl/xstULB
- Zabsonre P, Renambot J, Adoh-Adoh M, Coulibaly AO , Bertrand E. Conduction disorders in chronic parietal endocarditis or endomyocardial fibrosis. 170 cases at the Cardiology Institute of Abidjan. Dakar Med. 2000; 45: 15-19. Ref.: https://goo.gl/jKodw5
- Tamarappoo BK, John BT, Reinier K, Teodorescu C, Uy-Evanado A, et al. Vulnerable myocardial interstitium in patients with isolated left ventricular hypertrophy and sudden cardiac death: a postmortem histological evaluation. J Am Heart Assoc. 2012; 1: e001511. Ref.: https://goo.gl/DDHU7t
- Chugh SS, Kelly KL, Titus JL. Sudden cardiac death with apparently normal heart. Circulation. 2000; 102: 649-654. Ref.: https://goo.gl/xzMfy8
- Wilms HR, Midgley DJ, Morrow P, Stables S, Crawford J, et al. Evaluation of autopsy and police reports in the investigation of sudden unexplained death in the young. Forensic Sci Med Pathol. 2012; 8: 380-389. Ref.: https://goo.gl/WgzMNq
- Brunborg H. Befolkningen blir eldre. 2004. Ref.: https://goo.gl/1KvZVw
- Statistics Norway. Ref.: https://goo.gl/9WWvM8
- Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology. 2007; 18: 369-372. Ref.: https://goo.gl/NRFJCZ
- WHO. Ref.: https://goo.gl/nssAEN